Connect With Us
Blog
Items filtered by date: October 2024
Tuesday, 29 October 2024 00:00
How Diabetes Affects Wound Healing

Diabetes can significantly impair wound healing, particularly in the feet, where the risk of complications is higher. Elevated blood glucose levels in diabetic patients disrupt vital healing processes that delay tissue repair. For instance, diabetes often leads to poor circulation, which reduces oxygen and nutrient delivery to wound sites and further slows healing. Diabetic neuropathy, or nerve damage, makes it difficult for patients to feel foot injuries, which allows wounds to go untreated and increases the risk of infection. Meanwhile, the immune system is often weakened by this disease, making it harder for the body to fight infections that can further delay healing. Regular foot checks and early intervention are essential to managing foot wounds for people who are diabetic. If you have foot wounds that will not heal, it is suggested that you include a podiatrist as part of your medical team for treatment.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Carrie Frame, DPM from West Virginia Foot & Ankle. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Charleston, WV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Tuesday, 22 October 2024 00:00
What Is Haglund’s Deformity?

Haglund's deformity is a bony enlargement on the back of the heel bone, where the Achilles tendon attaches. This condition can cause significant discomfort and irritation, particularly where the heel rubs against the shoe. Symptoms typically include pain and swelling at the back of the heel, and in severe cases, the area may become red and tender. The primary cause of Haglund's deformity is often linked to wearing tight or rigid shoes, which can increase the pressure on the heel. Structural abnormalities in the foot or abnormal walking patterns may also contribute. Treatment focuses on relieving symptoms and preventing further irritation, although in some cases surgery may be needed. Conservative options include wearing well-fitted, cushioned shoes, using heel pads or orthotic inserts to reduce pressure, and performing stretching exercises for the Achilles tendon. For a more precise diagnosis and tailored treatment plan, it is suggested that you schedule an appointment with a podiatrist.
Many people suffer from bouts of heel pain. For more information, contact Carrie Frame, DPM of West Virginia Foot & Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in Charleston, WV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Tuesday, 15 October 2024 00:00
Medical Causes and Symptoms of Swollen Feet

Foot swelling, medically known as edema, occurs when excess fluid accumulates in the tissues of the feet. This condition can arise from various medical reasons, including heart failure, kidney disease, and venous insufficiency, where blood flow is impaired. It can also result from injuries, infections, or certain medications. Symptoms of foot swelling include noticeable puffiness, increased circumference of the foot, and discomfort or tightness in the affected area. In some cases, the swelling may be accompanied by pain or difficulty in movement. Identifying the underlying cause is vital for effective treatment and management. If your feet have become swollen, it is suggested that you confer with a podiatrist who can determine the cause and offer relief and treatment options.
Swollen feet can be a sign of an underlying condition. If you have any concerns, contact Carrie Frame, DPM of West Virginia Foot & Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Swollen feet are a common ailment among pregnant women and people who stand or sit for extended periods. Aging may increase the possibility of swollen feet and patients who are obese often notice when their feet are swelling too. There may be medical reasons why swollen feet occur:
- Phlebitis - A condition that causes the veins to become inflamed and can also cause leg pain.
- Liver disease - This may lead to low blood levels of albumin which is a protein. This can cause fluid in the blood to pass into the tissues and several areas of the body can become swollen.
- Heart failure - When the heart doesn’t pump properly the blood that is normally pumped back to the heart can pool in the veins of the legs causing swollen feet.
- Kidney disease - One of the main functions of the kidneys is releasing excess fluid in the body. This type of condition can make it difficult for the kidneys to function properly, and as a result the feet may become swollen.
- Deep-vein thrombosis (DVT)- This is a serious condition where blood clots form in the veins of the legs. They can block the return of blood from the legs to the heart which may cause the feet to swell. It is important to be treated by a podiatrist if this condition is present.
Swollen feet can also be caused by bone and tendon conditions, including fractures, arthritis, and tendinitis. Additionally, there may be skin and toenail conditions and an infection may cause the feet to swell. Patients who take medicine to treat high blood pressure may be prone to getting swollen feet.
Many patients elevate their feet to help relieve the swelling and this is generally a temporary remedy. When a podiatrist is consulted the reason behind the swelling can be uncovered and subsequently treated.
If you have any questions please feel free to contact our office located in Charleston, WV . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Tuesday, 08 October 2024 00:00
The Importance of Proper Toenail Trimming

Proper toenail care is key for preventing painful conditions like ingrown toenails. Trimming your toenails straight across, rather than rounding the edges or cutting them too short, helps prevent the nail from growing into the surrounding skin. This simple step is effective in avoiding ingrown toenails, which can be worsened by wearing shoes that are too narrow or short, causing your big toe to rub against the shoe. Initially, an ingrown toenail might not cause any symptoms, but over time, it can become painful, red, and swollen, and may even become infected with pus forming under the nail. To avoid these complications and ensure effective treatment, it is important to consult with a podiatrist. Early intervention can simplify the treatment process and alleviate discomfort more efficiently. If you are experiencing signs of an ingrown toenail, it is suggested you make an appointment with a podiatrist for professional care.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact Carrie Frame, DPM of West Virginia Foot & Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
- Improper toenail trimming
- Genetics
- Improper shoe fitting
- Injury from pedicures or nail picking
- Abnormal gait
- Poor hygiene
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our office located in Charleston, WV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Thursday, 03 October 2024 00:00
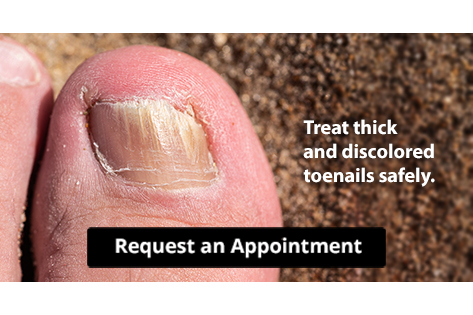
Stop Your Toenail Fungus
Tuesday, 01 October 2024 00:00
Nodules on the Sole of the Foot

Plantar fibromatosis, also known as Ledderhose disease, is a condition characterized by the growth of fibrous nodules, or fibromas, in the plantar fascia, the tissue on the sole of the foot. Its cause is not fully understood, but it is believed to be related to genetic factors, trauma, or repetitive stress on the feet. It is more common in individuals with other fibromatoses, such as Dupuytren’s contracture, a condition where the tissue under the skin of the palm thickens, causing the fingers, usually the ring and pinky, to curl inward over time. Diagnosis involves a physical exam where firm nodules can be felt under the skin. Imaging tests, such as ultrasound or MRI scans, may be used to assess the extent of the condition and rule out other issues like plantar fasciitis. Management typically begins conservatively with treatments like orthotics to relieve discomfort. In more severe cases, corticosteroid injections or surgery may be needed to remove the nodules, though recurrence rates can be high post-surgery. If you have a nodule on the bottom of your foot, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
A plantar fibroma may disrupt your daily activities. If you have any concerns, contact Carrie Frame, DPM of West Virginia Foot & Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Plantar Fibroma
A plantar fibroma is a fibrous knot in the arch of the foot. It is embedded in the plantar fascia which is a band of tissue that extends from the heel to the toes along the bottom of the foot. There can be multiple plantar fibromas in the feet at the same time. There are no known causes for this condition. If you have a plantar fibroma, there will be a bump in the arch of your foot that cannot be missed. Any associated pain is most often due to a shoe rubbing against the nodule. Non-surgical options, such as steroid injections, physical therapy, and orthotics should be tried first. Surgery is a last resort and is the only thing that will remove a plantar fibroma entirely. Consult with a podiatrist for a proper diagnosis and to determine the treatment regimen that is right for you.
What Causes a Plantar Fibroma?
While there are no specific causes identified, a plantar fibroma can possibly come from genetic predisposition or the formation of scar tissue that forms from healing the tears in the plantar fascia.
What Are the Symptoms of a Plantar Fibroma?
There will be a noticeable lump in the arch of the foot that may or may not cause pain. If pain is felt, it is typically because a shoe is rubbing up against the lump or when walking or standing barefoot.
Treatment and Prevention
A plantar fibroma will not disappear without treatment, but it can get smaller and be a non-issue. If pain persists, a podiatrist examines the foot and when the arch of the foot is pressed, pain can be felt down to the toes. An MRI or biopsy might be performed to help diagnose or evaluate the plantar fibroma. The following non-surgical options are generally enough to reduce the size and pain of these nodules:
- Steroid injections
- Orthotics
- Physical therapy to help apply anti-inflammatory creams on the bump
Surgery is considered if the mass increases in size and the patient continues to feel pain after non-surgical methods are tried.
If you have any questions please feel free to contact our office located in Charleston, WV . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.